Procedure Time: 30 minutes to 2 hours
Recovery Time: Minimal downtime, need to wear compression stockings for 2-3 weeks.
Results Duration: Permanent removal of varicose veins, long-lasting result.
Cost: Range from £1,900 to £4,500, depending on extent of treatment.
Anaesthesia: Local anaesthesia
For a full list of FAQs please Click Here.
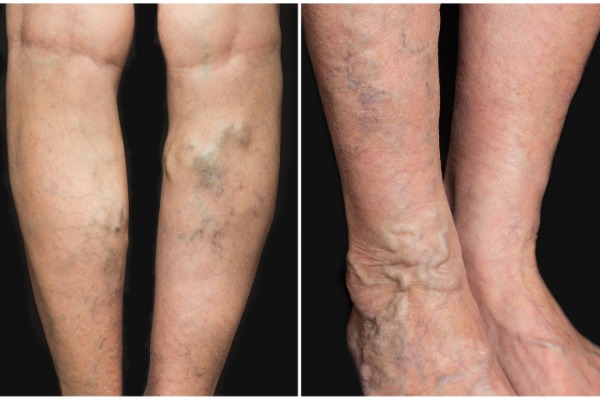
Endovenous Laser Ablation (EVLA), also sometimes marketed as Endovenous Laser Therapy™ (EVLT) is a minimally invasive method of treating varicose veins. It uses a laser which is inserted into the vein, guided by ultrasound scanning, under local anaesthetic to deliver heat energy which causes the vein to contract and seal itself shut. EVLA is used to treat an underlying venous reflux problem in veins higher up and deeper in the leg which are contributing to the presence of varicose and thread veins rather than treating the veins themselves. It is a ‘walk-in, walk out’ procedure so you will be able to leave the clinic after treatment. The cost of EVLA will depend on the number of varicose veins being treated, their severity and whether one or two legs are being treated. Private prices range from £1,900 up to approximately £4,500.
It is important to follow the advice of your vein specialist as closely as possible following EVLA to ensure that you get the full benefit of the treatment and avoid any complications.
Post-treatment advice may include: