
Beam me up, scalpel
AR in the OR: Boldly going where no surgery has gone before
Science fiction has become science fact as surgeons get set to use holograms to transform surgical procedures as we know them.
Researchers are set to present a study entitled Does augmented and mixed reality have a future role in reconstructive surgery? Exploring a potential application in mandibular reconstruction at the winter meeting of the British Association of Plastic, Reconstructive, and Aesthetic Surgeons (BAPRAS). The study shows how, in the near future, AR headsets could be worn by surgeons to project holographic images onto patients’ bodies during surgery, improving surgical precision and patient outcomes whilst reducing preoperative time.
The study, originally carried out at Princess Alexandra Hospital in Australia, focused on using the technology on 3D-printed models to test the feasibility of using AR (augmented reality) and MR (mixed reality) during mandibular (lower jaw) surgery. Researchers discovered that by using holograms instead of traditional physical cutting guides, they are able to display additional data, such as key anatomy information and surgical plans. In doing so, this may, in future, allow for more precision during surgery and save money by reducing preoperative planning time, decreasing turnaround time, and eliminating the need to print 3D cutting guides.
Resident medical officer Tyler Ferdinands, says, “Our early findings show that augmented and mixed reality has the potential to transform how surgeons plan and execute complex reconstructions. This preclinical pilot study demonstrates how AR/MR technology may improve efficiency while making complex anatomical details more accessible to the surgical team in real-time.”
The process is similar to traditional surgeries, with the primary difference being the use of holograms instead of physical cutting guides. The surgeon scrubs for surgery whilst wearing the headset and then scans the patient’s QR code to register the device. The software loads the holograms specific to that patient and projects them onto their body. For the study, participants used the Microsoft HoloLens 2 headset, which features tracking technology similar to that of gaming headsets like the Oculus Quest.

The holographic image of the patient anatomy includes details such as bone anatomy, blood vessels, an outline of the skin and surgical cutting planes. The final reconstruction is also displayed in the surgeon’s field of vision, allowing them to refer to it throughout the procedure.
Consultant plastic surgeon and BAPRAS president, Mani Ragbir, says, “This innovation aligns perfectly with our vision to advance surgical technology. By integrating AR/MR tools, we can equip surgeons with real-time, enhanced views that lead to safer, more efficient outcomes, particularly in complex cases like mandibular reconstruction. It is exciting to imagine AR as a significant part of the future of all surgery.”
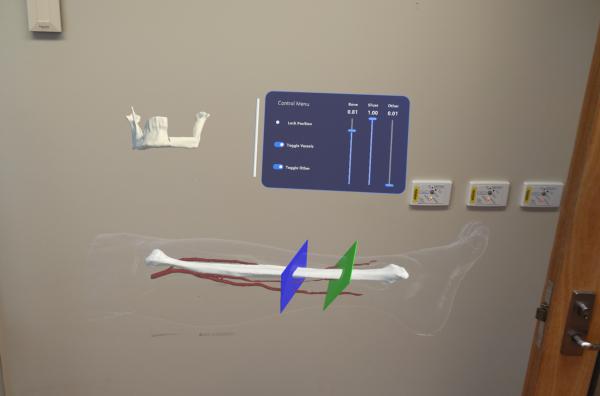
AR involves superimposing computer-generated images or data onto a real-world view. In the study, this meant projecting information onto a 3D-printed model, but it could be used on live patients in the future. These holograms allow surgeons to see essential details without looking away from the surgical site.
MR combines elements of both the real world and virtual environments, allowing for more interactive and immersive experiences. Surgeons can interact with virtual components as if they were part of their physical environment, manipulating digital elements in real time.
_(600_x_300_px)_(1).png)