Dermal filler-related blindness
Causes, prevention, and management
Dermal fillers have become one of the most widely used minimally invasive procedures in aesthetic practice. Although many have reported a recent downturn in dermal filler use in their practice, attributed to the rise in popularity of regenerative procedures, the global dermal fillers market is still extensive, valued at $5.08 billion USD in 2023 and projected to grow to $10.16 billion by 2032.1
Despite their generally safe profile, complications such as blindness, though rare, are among the most severe outcomes. Understanding the mechanisms, preventive strategies, and treatment options for dermal filler-induced blindness is crucial for practitioners in aesthetic medicine.2
Understanding the mechanism of blindness from fillers
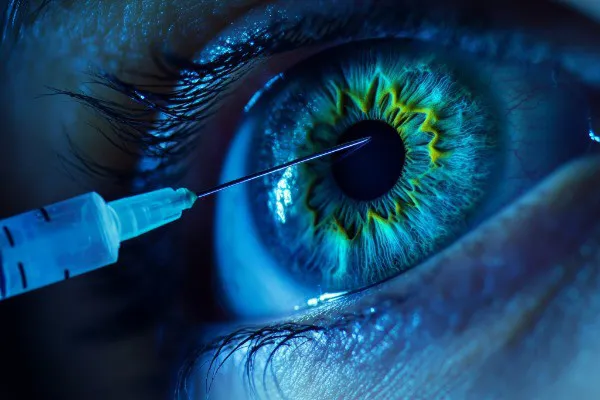
Blindness caused by dermal fillers occurs due to vascular occlusion. When filler material, most commonly hyaluronic acid – 76% of cases according to a 2024 literature review2 – is inadvertently injected into or compresses an arterial vessel, it can cause retrograde embolisation. The filler can travel to the ophthalmic artery or its branches, leading to retinal artery occlusion (RAO) and subsequent visual loss.
Key studies, such as those by Lazzeri et al. (2012)3 and Kim EG et al. (2014)4, have demonstrated that even small volumes of filler injected into high-risk areas such as the glabella, nasal dorsum, or periorbital region can lead to blindness. Anatomical variations and high vascular density in these areas increase the risk of complications.
Risk areas and procedural considerations
Certain facial zones are considered high risk for vascular compromise. These include:
- Glabella: Injection into the supratrochlear or supraorbital arteries.
- Nasal dorsum: Connection with the angular and ophthalmic arteries.
- Periorbital region: Proximity to arterial branches supplying the retina.
In April 2024, a literature review was performed to identify all cases of visual complications caused by filler injection published between September 2018 and March 2023. It identified the sites that were the highest risk were the nose (40.6%), forehead (27.7%), and glabella (19.0%).
Practitioners must have an in-depth knowledge of facial anatomy to avoid these regions or employ safer techniques.
Preventive strategies
To mitigate the risk of dermal filler-related blindness, adherence to the following best practices is essential:
- Comprehensive training: Clinicians must undergo specialised training in dermal filler administration and complications management. Understanding vascular anatomy and high-risk zones is critical.
- Aspiration before injection: Aspiration prior to injecting filler can help identify if the needle is within a blood vessel, although this is not foolproof.
- Use of cannulas: Blunt-tip cannulas reduce the likelihood of penetrating blood vessels compared to sharp needles.
Slow injection and minimal pressure: Slowly injecting small amounts of filler minimises the risk of embolisation. - Patient positioning: Proper positioning of patients during the procedure ensures optimal visibility and safety.
- Real-time communication: Encouraging patients to report any pain or visual disturbances during the procedure can help identify early signs of vascular occlusion.
Early recognition and treatment of complications
Blindness due to filler embolism is typically sudden and often accompanied by severe pain or other visual symptoms.
The most common associated signs were ptosis (56.2%), ophthalmoplegia (44.1%), pain (31.2%), and blanching and other skin changes (73.2%).2 Nausea and headache may also occur.2 Strokelike features were seen in 19.2% of cases. 2
Early recognition is vital, as delays in treatment significantly reduce the chances of recovery. If you suspect a visual complication, stop injecting immediately.2
Management of dermal filler blindness
Filler-related blindness is an ophthalmologic emergency. The goal of treatment is to recanalise the vessel and reperfuse tissue.2 The most cited time window for reperfusion is 90 minutes.5 However, newer literature suggests it may be as little as 10 to 15 minutes, emphasising the need for immediate recognition and management.6
The Aesthetic Surgery Journal review has a downloadable emergency guide.2 It recommends establishing a filler-induced blindness protocol and always having an abundant supply of nonexpired hyaluronidase on hand.2,7
It suggests having a pre-established relationship with an ophthalmologist or oculoplastic surgeon and, before starting treatment, briefly examine each eye separately and document:
- Pupillary response to light
- Extraocular muscle function
- Visual acuity
Hyaluronidase injections
If hyaluronic acid filler has been used, hyaluronidase can be injected at the original filler treatment site, anywhere with skin ischemia, and along the arterial pathways leading to the eye.2 Subcutaneous injections of hyaluronidase (HYAL) at the filler injection site were reported to be the preferred method of management in 70% of cases in the most recent review of the data.2
The enzyme hyaluronidase breaks down hyaluronic acid and can restore blood flow when administered promptly.
Key considerations for hyaluronidase injections:
- Administer within hours of the onset of symptoms.
- Performed by trained professionals to minimise risks.
The technique now favoured is the supraorbital method.
“Injectors are encouraged to attempt supratrochlear and supraorbital injections, with which hyaluronidase is injected adjacent to and inside the supraorbital and supratrochlear notches.”2
Subcutaneous injections of HYAL at the original injection site, along the path of the vessels, and around the supratrochlear and supraorbital artery notches or foramina are non-invasive and easy to carry out immediately at the bedside.
The review showed retrobulbar injections only demonstrated success in 5.3% of attempts and noted that its use “remains controversial”, adding, “recent papers suggest this technique is unlikely to be helpful and should only be attempted by physicians familiar with this treatment.”2,8,9,10,11
“The supraorbital method involves injecting hyaluronidase into the supraorbital foramen, specifically into the supraorbital artery, which is located above the eyebrow”, explains Dr Patrick Treacy, who proposed the supraorbital route instead of the retrobulbar one back in 2013.12-14 “This method requires no special skills, is less invasive than the retrobulbar method and can be effective in cases where the blood vessel blockage is closer to the surface of the skin.”15
This technique is also supported in the ACE Group World Guidance, which reads: “Based on the current evidence regarding retrobulbar injections of hyaluronidase, the Aesthetic Complications Expert Group do not advocate this treatment for visual loss caused by hyaluronic acid filler. Injection of hyaluronidase into the supratrochlear or supraorbital arteries to reach the embolus seems a more sensible approach.” 16
In addition, recent literature indicates that increased ocular venous pressure may open arteriovenous shunts in the periorbital area, which may be advantageous when flooding this area with hyaluronidase.2,17
A groundbreaking case study by Nguyen et al. (2022)18 highlights the potential for significant vision recovery from filler-induced blindness using a combined approach of intra-arterial hyaluronidase and thrombolytic agents. The case involved a 27-year-old female who experienced total vision loss and severe ocular symptoms following a 1.0 mL hyaluronic acid filler injection in the nasal dorsum. Prompt multidisciplinary intervention led to remarkable results.
Subcutaneous and retrobulbar hyaluronidase injections were initially administered, followed by intra-arterial hyaluronidase injections guided by digital subtraction angiography (DSA).
Despite partial recovery, a secondary occlusion occurred 13 hours later, leading to the use of intra-arterial thrombolysis with alteplase, a thrombolytic agent, combined with hyaluronidase.
Post-treatment, the patient’s vision improved significantly from no light perception (NLP) to 20/50 within three months.
The success achieved suggests that advanced techniques such as intra-arterial thrombolysis can be lifesaving in select cases.
Hyperbaric Oxygen Therapy (HBOT)
Hyperbaric oxygen therapy can enhance tissue oxygenation and promote recovery in cases of partial ischemia. However, its efficacy is limited when used as a standalone treatment.
The Aesthetic Surgery Journal review2 showed that 29 cases underwent hyperbaric oxygen therapy, with 12 (41.4%) experiencing improvements in vision, including five that recovered normal vision. The authors wrote: “It should be noted that hyperbaric oxygen was co-administered with other treatments, such as IATT and advanced HYAL rescue techniques (e.g., retrobulbar or supratrochlear injections). A total of 20 cases (6.6%) had anterior chamber puncture or paracentesis. Across studies, dozens of other management strategies were attempted, including ocular massage, aspirin, anticoagulants, acetazolamide, eye drops, nitroglycerin, antibiotics, mannitol, and prostaglandins.”
Alternative Interventions
The ACE Group World Guidance16 outlines other supportive therapies as:
- Anterior chamber paracentesis to immediately lower intraocular pressure.
- Steroid administration, intravenous dexamethasone
- Judicious use of antibiotics for suspected infection
- Intravenous prostaglandin E14 to increase blood flow to the retina and decrease activation of thrombocytes and neutrophils.
Long-term outlook and ethical considerations
Blindness following dermal filler procedures often results in permanent visual loss, profoundly impacting patients’ quality of life. This underscores the importance of patient education, informed consent, and adherence to safety protocols. Practitioners must ensure that patients are fully aware of the potential risks, even if rare.
Conclusion
While dermal fillers remain a popular and largely safe cosmetic option, the risk of blindness is a stark reminder of the importance of procedural expertise, knowledge of anatomy, and prompt management of complications. Ongoing research and improved techniques will continue to enhance the safety of these procedures. By adhering to best practices and remaining vigilant, practitioners can minimise risks and ensure better outcomes for their patients.
You can watch Dr Patrick Treacy’s lecture on dermal filler blindness to the Royal College of Ophthalmology here: https://www.youtube.com/watch?v=A4rg-ExCWEo
You can download ACE Group World’s guidance on Vision Loss Secondary to Cosmetic Filler Injection here: https://uk.acegroup.online/wp-content/uploads/2020/10/ACE-Group-Visual-Loss-v2.7.pdf
References
- Fortune Business Insights, Dermal Fillers Market Size, Share & Industry Analysis. Accessed December 12, 2024. https://www.fortunebusinessinsights.com/industry-reports/dermal-fillers-market-100939
- Valerie C Doyon, Chaocheng Liu, Rebecca Fitzgerald, Shannon Humphrey, Derek Jones, Jean D A Carruthers, Katie Beleznay, Update on Blindness From Filler: Review of Prognostic Factors, Management Approaches, and a Century of Published Cases, Aesthetic
- Surgery Journal, Volume 44, Issue 10, October 2024, Pages 1091–1104, https://doi.org/10.1093/asj/sjae091
- Lazzeri D, Agostini T, Figus M, Nardi M, et al, Blindness following cosmetic injections of the face. Plast Reconstr Surg 2012;129: 995–1012.
- Kim EG, EOM TK, Kang SJ, Severe visual loss and cerebral infarction after injection of hyaluronic acid gel. J Craniofac Surg 2014;25:684–6.
- Hayreh SS, Zimmerman MB, Kimura A, Sanon A. Central retinal artery occlusion. Retinal survival time. Exp Eye Res. 2004;78(3):723–736. doi: 10.1016/S0014-4835(03)00214-8
- Tobalem S, Schutz JS, Chronopoulos A. Central retinal artery occlusion-rethinking retinal survival time. BMC Ophthalmol. 2018;18(1):4–9. doi: 10.1186/s12886-018-0768-4
- Jones DH, Fitzgerald R, Cox SE, et al. Preventing and treating adverse events of injectable fillers: evidence-based recommendations from the American society for dermatologic surgery multidisciplinary task force. Dermatologic Surg. 2021;47(2):214–226. doi: 10.1097/DSS.0000000000002921
- Taylor GI, Shoukath S, Gascoigne A, Corlett RJ, Ashton MW. The functional anatomy of the ophthalmic angiosome and its implications in blindness as a complication of cosmetic facial filler procedures. Plast Reconstr Surg. 2020;146(4):745. doi: 10.1097/PRS.0000000000007155
- Goodman GJ, Magnusson MR, Callan P, et al. A consensus on minimizing the risk of hyaluronic acid embolic visual loss and suggestions for immediate bedside management. Aesthetic Surg J. 2020;40(9):1009–1021. doi: 10.1093/asj/sjz312
- Martel A, Lagier J, Sarfati E, et al. Filler-induced blindness “seen” by ophthalmologists: case presentation and treatment algorithm. J Fr Ophtalmol. 2022;45(7):771–783. doi: 10.1016/j.jfo.2022.03.005
- Lei Z, Qingyi Z, Hong X, et al. Long-term prognosis of vision loss caused by facial hyaluronic acid injections and the potential approaches to address this catastrophic event. Aesthetic Surg J. 2023;43(4):484–493. doi: 10.1093/asj/sjac329
https://www.linkedin.com/pulse/dr-patrick-treacy-discusses-dermal-filler-how-deal-them-treacy/ - Treacy P, Facing complications. Body Language 2015;77:20 6.
- https://www.youtube.com/watch?v=9xs9AGGm2dQ
- Reversing dermal filler blindness | June 2023 - Aesthetic Medicine Magazine
- https://uk.acegroup.online/wp-content/uploads/2020/10/ACE-Group-Visual-Loss-v2.7.pdf
- Wang Y, Li Q, Ye Y, et al. Intra-arterial thrombolytic treatment for visual deficits caused by hyaluronic acid filler: efficacy, safety, and prognostic factors. Plast Reconstr Surg. 2023;152(6):1226–1233. doi: 10.1097/prs.0000000000010374
- Nguyen HH, Tran HTT, Duong QH, Nguyen MD, Dao HX, Le DT. Significant Vision Recovery from Filler-Induced Complete Blindness with Combined Intra-Arterial Injection of Hyaluronidase and Thrombolytic Agents. Aesthetic Plast Surg. 2022 Apr;46(2):907-911. doi: 10.1007/s00266-021-02658-w. Epub 2021 Nov 12. PMID: 34767060.
