CPD: The Regenerative Power of DHEA
Miriam Martinez Callejas, Superintendent Pharmacist and co-founder of Roseway Labs, unveils the role of DHEA in human tissue rejuvenation.
Tissue regeneration is a complex and highly regulated process involving the replacement of damaged or dead cells with new, functional ones. It plays a pivotal role in maintaining the health and vitality of various tissues, including skin, muscle, bone and organs. As we age, cells naturally experience damage and get depleted, and by restoring these, our health benefits in a number of ways.
In this 15-minute article, we will explore the potential of DHEA to rejuvenate various tissues in the human body, starting with the effects that DHEA can have on bodily tissue. We will then look at how it may deliver these results and other benefits that may be realised. Finally, we will touch on the available forms of DHEA and its safety as a medication.
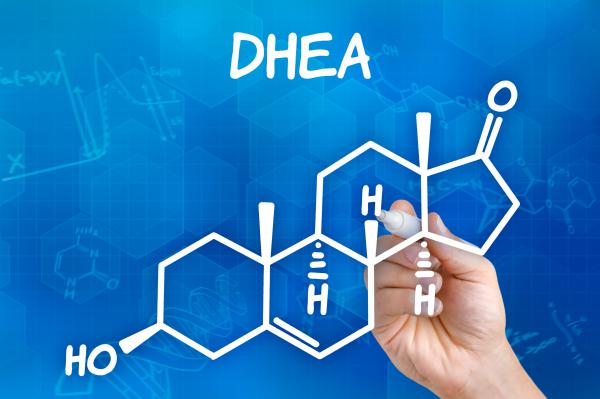
Dehydroepiandrosterone (DHEA) is an androgenic steroid hormone primarily produced by the adrenal glands and in smaller quantities by the brain and the gonads. It converts in the body to the sex hormones testosterone and oestrogen, but its role extends far beyond that of a simple hormone precursor.
Taking DHEA rather than oestradiol and testosterone can reduce some of the side effects produced by HRT. As the body converts DHEA into smaller quantities of sex hormones, the approach is more gentle and better tolerated by people with sensitivities.
DHEA, also known as prasterone, is a controlled drug (Section 4, Class II) in the UK and can only be obtained via a prescription. It is not a food supplement and is a medication that must be prescribed by a qualified medical practitioner. There is one UK-licensed medication containing DHEA – Intrarosa – which is licensed for vulvar and vaginal atrophy. Roseway Labs offers many forms of DHEA, such as capsules, pessaries, troches, gels and creams as compounded and manufactured unlicensed medication.
DHEA topical formulations have been explored for their potential to improve skin health, including reducing signs of ageing, increasing dermal thickness and enhancing skin elasticity1. These effects are thought to be related to DHEA’s influence on both collagen synthesis and hyaluronic acid synthesis, which improve skin hydration. Enhanced moisture retention can lead to smoother and more supple skin. Whilst a topical dose would be significantly lower than an oral dose, there is still a chance that the DHEA is systemically absorbed through the skin, and this must be considered before prescribing.
DHEA taken orally may promote the repair of damaged skin tissue in wounds by accelerating the proliferation of skin cells and the formation of new blood vessels (angiogenesis), which is essential for tissue regeneration. These vessels deliver oxygen, nutrients, and immune cells to the regenerating tissue, facilitating the healing process.
In postmenopausal women, DHEA has been used to address issues related to vaginal atrophy and vaginal dryness. DHEA’s local effects on the vaginal mucosa have been reported as increasing lubrication, thickening the local tissue and, as a result, reducing pain and the likelihood of infection. Whilst DHEA pessaries are often used to treat vaginal atrophy, in severe cases, the pessary does not sufficiently stick to the vaginal tissues for the duration of the treatment, and it can
be more beneficial to use a muco-adhesive gel or cream.
Studies have suggested that oral DHEA may have a modest effect on bone density in postmenopausal women. Tissue regeneration in bone is one factor, with an added benefit of the breakdown of DHEA into testosterone and oestrogen, both of which play a crucial role in maintaining bone density.
DHEA, as opposed to its metabolites of testosterone and oestrogen, acts to regenerate tissue in three physiological ways.
Immune Modulation: DHEA has been shown to have immunomodulatory effects, which could indirectly influence tissue regeneration by reducing inflammation and promoting a balanced immune response that effectively responds to tissue damage without excessive inflammation or immune suppression.
Metabolism: DHEA is known to affect metabolism and energy levels, which can indirectly support tissue repair and regeneration by providing the necessary nutrients and energy for cellular processes. Improved metabolism ensures that tissues receive adequate nutrients for regeneration. DHEA may increase insulin sensitivity in diabetic or pre-diabetic patients. Studies have suggested it can also modulate insulin-signalling pathways and enhance glucose uptake in adipose tissue.
Antioxidant Activity: DHEA possesses antioxidant properties, which means it can help neutralise harmful free radicals in the skin and reduce oxidative stress. Free radicals can damage skin cells and accelerate the ageing process.
Other suggested benefits of DHEA include cell proliferation, lower inflammation, enhanced collagen production, vasodilation and increased metabolic function.
DHEA has been shown to stimulate cell proliferation, particularly in tissues with a high turnover rate, such as the skin and mucous membranes. Cell division replaces damaged or dead cells with new, functional ones and by promoting the growth and replication of cells, DHEA contributes to the regeneration of damaged tissues.
Chronic inflammation can hinder tissue regeneration. DHEA’s anti-inflammatory properties help reduce inflammation, creating a more conducive environment for tissue repair.
Collagen is a crucial component of connective tissues like skin and tendons and a key structural protein in the skin that provides strength and elasticity. DHEA has been linked to increased collagen production, aiding in tissue repair and rejuvenation, and it appears to stimulate the production of collagen in the skin. This effect can contribute to improved skin firmness and a reduction in the appearance of fine lines and wrinkles.
Vasodilation, the widening of blood vessels, plays a vital role in tissue health and regeneration. Adequate blood flow ensures that tissues receive the necessary nutrients and oxygen for optimal function and repair whilst also facilitating the removal of waste products. DHEA has been associated with improved vasodilation and vascular endothelial function through several mechanisms, particularly nitric oxide production, which relaxes blood vessel walls. This effect can also help regulate blood pressure, reducing the strain on the cardiovascular system and improving overall tissue health.
The safety of taking DHEA either individually or as part of hormone replacement therapy depends on various factors, including the patient’s medical history, the dosage used and the duration of use. Using it at high doses or for extended periods without proper supervision can lead to androgenic side effects and potential health risks. Clinicians should always monitor hormone levels to ensure they are within a safe and balanced range.
DHEA can be administered orally, vaginally or topically. Oral DHEA is convenient and works systemically but can be associated with variable absorption rates and potential first-pass metabolism effects, where stomach acid and liver detoxification reduce the bioavailability of the medication. Often, oral doses of medication are higher in order to counter this effect. Vaginal DHEA pessaries, gels or creams allow for targeted delivery to the vaginal and pelvic tissues, with the aim of acting on the vaginal membranes for an extended period of time. Topical DHEA creams or gels can provide localised effects on the skin. This method offers control over the application site but may require consistent use for optimal results.

Did you find this article useful?
Send your follow-up questions to info@rosewaylabs.com or visit them at rosewaylabs.com
