
CPD Article: Beyond the Surface
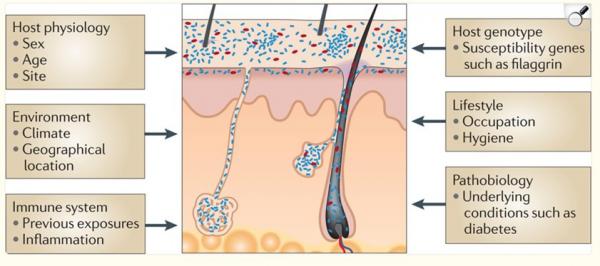
The microbiome is the collective term for the trillions of bacteria, viruses, fungi, and other microorganisms that inhabit the human body. It begins to develop at birth. Whether a baby is delivered vaginally or by caesarean section, and whether they are breastfed or formula-fed, has a significant influence on the initial microbial composition. From there, the microbiome continues to evolve throughout life, shaped by diet, hormone levels, medications (particularly antibiotics), lifestyle, environment, and stress.
These microbes play a vital role in digestion, hormone regulation, immune function, and, importantly for us, skin health.
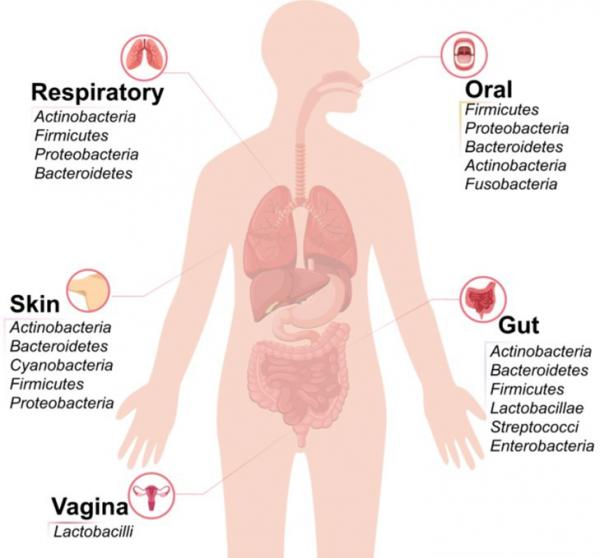
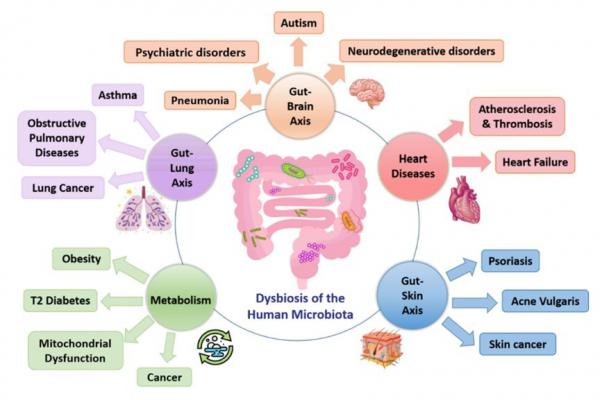
There are five main microbiome reservoirs in the body: the gut, skin, oral cavity, respiratory tract, and genitourinary tract. These sites are not isolated. They interact with one another through immune signalling, metabolic products, and the nervous system. One key example of this interaction is the gut–skin axis, which refers to the bidirectional communication between the gastrointestinal system and the skin.
What is dysbiosis?
Dysbiosis refers to an imbalance in the microbial communities that live within or on the human body, most commonly in the gut or on the skin. In a healthy state, these microorganisms exist in harmony, supporting barrier function, regulating inflammation, and contributing to overall wellbeing. However, when this balance is disrupted, it can lead to an overgrowth of harmful bacteria, a reduction in beneficial strains, and an increase in inflammatory signalling.
Several factors can contribute to dysbiosis, including:
- Frequent or prolonged antibiotic use
- Diets high in processed foods and low in fibre
- Chronic psychological stress
- Hormonal changes
- Environmental toxins
- Harsh or overly sterile skincare products
Dysbiosis has been linked to many health problems.
Skin microbiome
Skin microbiome is a relatively stable ecosystem. It acts as a barrier against pathogens. Staph ep, P. acne, Corynebacterium, Malassezia and Dermodex are the most common spaces. Dysbiosis in the skin microbiome is responsible for many chronic inflammatory skin conditions, such as acne, rosacea, eczema, psoriasis, and impaired healing, particularly after aesthetic treatments like microneedling, laser, or injectables.
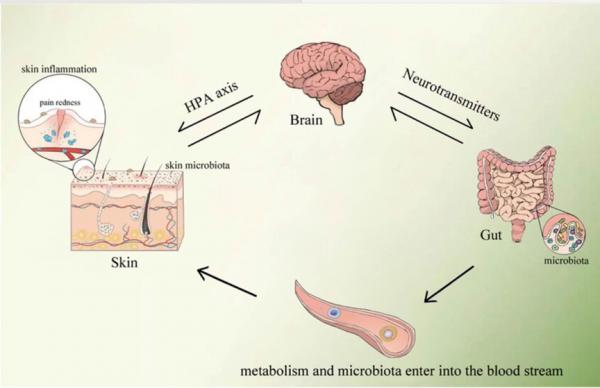
The Gut–Brain–Skin Axis
While the gut–skin axis highlights the connection between digestive health and skin condition, it’s now evident that the brain plays a critical role in this relationship as well. Both acute and chronic stress can affect gut and skin function, but chronic stress appears to have a more prolonged and disruptive impact on the microbiome. One proposed mechanism involves activation of the hypothalamic–pituitary–adrenal (HPA) axis, leading to elevated cortisol levels.
This hormonal response contributes to chronic inflammation, weakens immune function, and disrupts the balance of the gut and skin microbiomes. It can also lead to bowel dysfunction, such as bloating, altered motility, and increased intestinal permeability, all of which further contribute to systemic inflammation and skin flare-ups. These changes may result in increased sensitivity, acne, eczema flares, and delayed recovery after aesthetic procedures.
Prebiotics, probiotics and postbiotics
As awareness of the microbiome grows, patients are increasingly asking about supplements, skincare, and diet changes that claim to support it. For aesthetic practitioners, understanding the differences between prebiotics, probiotics, and postbiotics is essential.
Prebiotics are non-digestible fibres that act as food for beneficial bacteria. By nourishing the microbiome, they help promote microbial diversity and reduce inflammation. In skincare, the most commonly used prebiotics are inulin, alpha-glucan oligosaccharide, and xylitol. These ingredients help selectively nourish the skin’s beneficial bacteria and enhance its barrier function. They are currently found in many over-the-counter moisturisers, serums, and cleansers designed for sensitive or microbiome-friendly skin.
Probiotics are live microorganisms – typically beneficial strains of bacteria – that offer health benefits when consumed or applied in the right amounts. In skincare, incorporating live probiotics is technically challenging due to stability issues. At Hardwick Clinic, we use the Esse Skincare Live Probiotic Serum, which contains encapsulated live strains of Lactobacillus. Other brands offering live probiotic skincare are beginning to emerge, reflecting growing demand and innovation in this space.
As the Western diet is often low in fibre and fermented foods, oral supplementation with probiotics and prebiotics is increasingly popular. This can be particularly helpful in individuals with signs of dysbiosis, poor dietary habits, or chronic inflammation. In these cases, oral supplementation may support not only gut health but also improve skin clarity, barrier repair, and post-treatment recovery — especially when used as part of a broader in-clinic skincare programme.
Probiotics are produced using two methods:
- Isolated strain fermentation, which allows for precise control of clinically studied strains, standardised dosing, and strain-specific benefits.
- Natural or multi-strain fermentation, where a diverse microbial community is grown together in a food base over several years, producing a broad spectrum of bacteria and postbiotic compounds.
At Hardwick Clinic, we use Dr Ohhira’s Probiotics, which are made using the natural fermentation method and contain a blend of prebiotics, probiotics, and postbiotics in a single capsule.
Postbiotics are bioactive compounds produced when probiotics metabolise prebiotics. These include short-chain fatty acids, enzymes, peptides, and cell wall fragments. In skincare, lactobacillus ferment lysate and bifida ferment lysate are widely used for their soothing, anti-inflammatory, and barrier-repairing properties. Postbiotics are shelf-stable and easy to formulate, making them ideal for calming sensitive or post-treatment skin.
Stress management and the gut–brain–skin axis
Stress is a critical , yet often overlooked, factor in skin health. Through the gut–brain–skin axis, psychological stress can disrupt both gastrointestinal and dermatological balance. Chronic stress activates the HPA axis, raises cortisol levels, alters microbiome composition, and increases inflammation. These changes can result in skin flares, heightened sensitivity, and slower healing – all highly relevant to aesthetic medicine.
At Hardwick Clinic, we incorporate practical, accessible stress-management strategies into our patient care model:
- We share the Action for Happiness calendar each month via our newsletter, encouraging simple, daily actions that boost mood and connection.
- We advise the 4-7-8 breathing technique, a quick and effective tool for calming the nervous system. This method of breathing is good for the management of anxiety, stress, sleep, and overall wellbeing.
By addressing stress alongside skin and gut health, we can significantly enhance patient outcomes and satisfaction.
Conclusion
The gut–brain–skin microbiome axis provides a compelling clinical model that unites gut health, mental wellbeing, and skin as part of the whole-body holistic approach to longevity. As research evolves, so too must our approach to aesthetic care. By recognising the role of the microbiome and stress in treatment response and skin rejuvenation, we can deliver better and more personalised results.
Supporting patients through dietary advice, appropriate supplementation, microbiome-friendly skincare, and emotional wellbeing is no longer a luxury – it’s a vital extension of modern aesthetic practice.
References
- Portman DJ, Gass ML; Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and The North
- American Menopause Society. Menopause. 2014 Oct;21(10):1063–1068.
- Faubion SS, Larkin LC, Stuenkel CA, et al. Management of genitourinary syndrome of menopause in women with or at high risk for breast cancer: consensus recommendations from The North American Menopause Society. Menopause. 2018 Apr;25(4):596–608.
- Pastor Z, Hlavackova M, Uzel R. Impact of genitourinary syndrome of menopause on quality of life. Int J Environ Res Public Health. 2022;19(13):7617.
- MacBride MB, Rhodes DJ, Shuster LT. Vulvovaginal atrophy. Mayo Clinic Proceedings. 2010 Jan;85(1):87–94.
- Di Pietro S, Russo R, Gennari R, et al. Vulvar rejuvenation with Polynucleotides HPT and benefits on postmenopausal sexual life disruption.Obstetrics & Gynecology Research. 2022;6(3):1–7.
- Palmieri B, Rottigni V, Iannitti T. Preliminary study of polynucleotide skin applications in aesthetic medicine. Dermatol Ther. 2014 May-Jun;27(3):143–147.
- Palmieri B, Capone S, Capone G, et al. Polynucleotides and hyaluronic acid: a new dermal biorevitalization treatment. J Cosmet
- Dermatol. 2019 Jun;18(3):896–901.
- Casabona F. Use of polynucleotides associated with hyaluronic acid for vulvovaginal rejuvenation in menopause: a pilot study. Eur Rev Med Pharmacol Sci. 2022 Apr;26(7):2603–2610.
_(600_x_200_px).jpg)
.png)